|
|
PROJECTS
Innovation Lab @ Semel Institute
I started and direct the Innovation Lab, supported by the Semel Institute for Neuroscience and Human Behavior and the Center for Health Services and Society. The Innovation Lab works to support a partnered, multidisciplinary approach to fostering research and healthcare innovation through participatory research methods, translational science, and technology. The central technology that powers the lab is Chorus, a participatory technology platform that enables people without technical expertise to create their own mobile interventions (see below). Efforts span predictive analytics, telehealth and mobile, behavioral biomarkers, and healthcare redesign.
Importantly, in all these efforts we implement key principles of participatory research including a focus on equity, trust, transparency, respect, knowledgesharing, and shared control across a broad group of stakeholders including patients, community leaders, health system administrators, policy makers, and more. The projects below are various examples of how these have come together in practice so far... CHORUS
What happens when everyone can be an app developer? How does that change what gets created? How does it impact equity, relevance, impact, and sustainability of digital technologies?
These are the motivating questions behind Chorus - a web application I created that provides a simple, visual interface to create mobile web and interactive text message and voice apps. Only 0.1% of the population is a computer programmer. That leaves 99.9% of the population out of the conversation when it comes to actually creating technologies. And who creates matters. The goal with Chorus is to support 100% of the population to create digital technologies - because everyone is an expert from their own lived experience. Now, individual experts with knowledge of their own experiences, challenges, and strengths and that of their communities can create, iterate and sustain technologies that are important for them. Chorus is a HIPAA-compliant, hosted service from the Innovation Lab. It currently supports over 30 projects at various universities as well as local agencies such as Los Angeles Unified School District and Healthy African American Families. 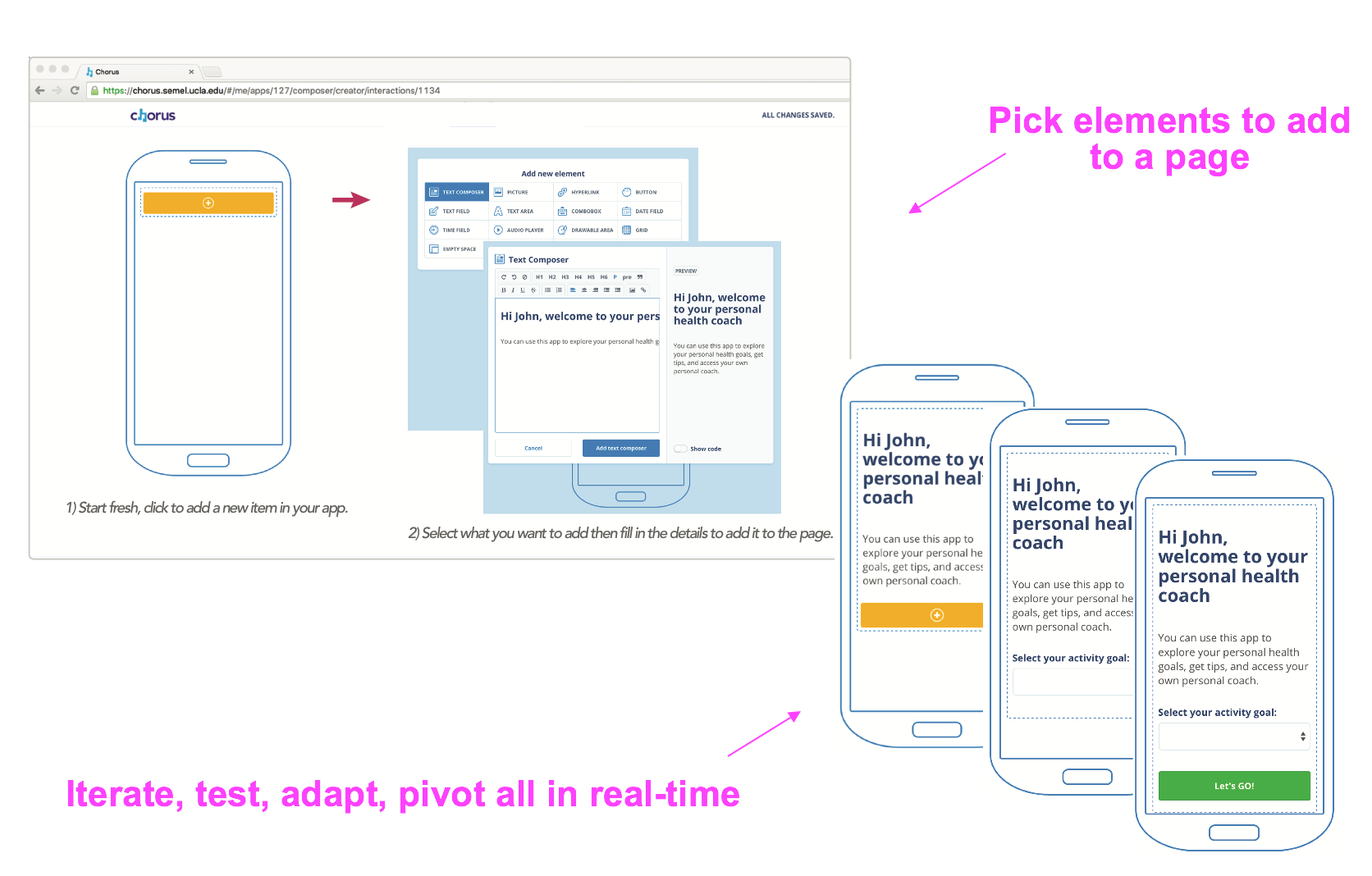
References B-RESILIENT: Communities as app creators
The B-RESILIENT project builds on the Chorus platform and combines it with Community-Partnered Participatory Research principles to facilitate participatory technology development with our community partners including Health African American Families in South Los Angeles. We conducted a series of partnered workshops to co-create over a period of months a resiliency-focused text messaging app that was adapted from an existing manual in PDF form (Building Resilience in Communities for Health - B-RICH). Through this process, we identified togetehr key concepts to focus on relevant to community needs, adapted the language both for the short form of text messages but also to improve accessibility. This was an iterative process with small pilots followed by subsequent changes/improvements. We recently completed a pilot randomized controlled trial of the app as well. Oh, and we had fun making it! (if you can tell from pics below)

References
Personal Health Apps: Patients as app creators
This project takes an extreme view of what it means to be involved in your treatment as a patient! In partnership with the UCLA Partial Hospitalization and Intensive Outpatient Treatment Programs, we have implemented Chorus to support individual patients and their providers to co-create togehter their own mobile apps to support their care - and then use them in real-time. Every patient has a unique set of goals, challenges and strengths related to their care, and those change over time as treatment progresses. Now, patients and their therapists create apps that are customized to those needs - at the individual level! So each app is unique to that patient, and changes over time as their needs change. This supports a truly patient-centered approach to care and the technology that supports it. The goal is to help patients engage more in their care and implement skills in their daily lives for improved outcomes - both related to their symptoms as well as quality of life and functioning. We are currently conducting a randomized controlled trial at UCLA. Publication of pilot results coming soon! Currently under review...
Individual-level, "micro" apps for patients 
MyCoachConnect: Predictive analytics and behavioral biomarkers
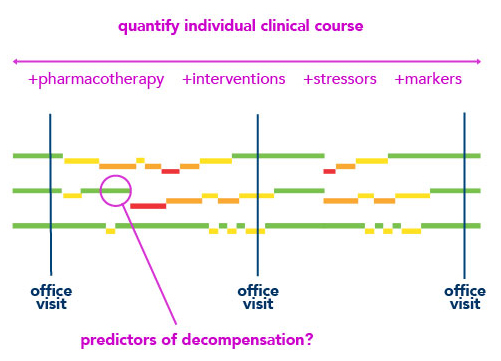 Personalized and predictive mental health through a novel, mobile engagement tool using participatory engagement techniques and machine learning. This area encompasses several related efforts. The main one is "MyCoachConnect" - an interactive voice response system that uses patient-recorded voice samples to predict mental heatlh states over time. Individuals have varying courses related to their symptoms and mental health states and most serious mental illnesses like schizophrenia, bipolar and major depression have recurrent symptoms as well as periods of stability. It is currently very difficult to know at an early stage when mental health states change or to predict future changes. However, with early detection, we could support early interventions that could potentially improve outcomes for individuals and prevent decompensation. Publication of pilot results coming soon! Currently under review...
Personalized and predictive mental health through a novel, mobile engagement tool using participatory engagement techniques and machine learning. This area encompasses several related efforts. The main one is "MyCoachConnect" - an interactive voice response system that uses patient-recorded voice samples to predict mental heatlh states over time. Individuals have varying courses related to their symptoms and mental health states and most serious mental illnesses like schizophrenia, bipolar and major depression have recurrent symptoms as well as periods of stability. It is currently very difficult to know at an early stage when mental health states change or to predict future changes. However, with early detection, we could support early interventions that could potentially improve outcomes for individuals and prevent decompensation. Publication of pilot results coming soon! Currently under review...
Equity, trust and digital dispairities However, along with this comes important issues related to the machine learning and predictive algorithms as well as the personal data they use. It goes beyond keeping data private. For example, algorithms can be very sensitive to biases in the data used to train them which can lead to uneven performance/benefit/risk across different socioeconomic groups. That's why we combine this novel approach from a technical perspective with participatory research methods to support an evolving process that emphasizes equity, trust, respect and shared control/benefit. By doing so, we hope explore ways to avoid creation of a new digitial divide and worsening of existing disparities related to health and social determinants of health. C-LEARN: Community Resilience Learning Collaborative and Research Network
 This is a partnered project between Lousiana State University and UCLA funded by the National Academies of Science and Robert Wood Johnson Foundation. Dr. Benjamin Springgate at Louisiana State University is the overall Principal Investigator (PI) and I'm the PI for UCLA. Community Resilience Learning and Collaborative and Research Network (C-LEARN) is about better understanding the capacity to address resilience to disasters, hurricanes, storms, floods, oil spills and other natural or man-made catastrophes. We use community-partnered participatory research (CPPR) to engage stakeholders and evaluate effects of interventions on community and individual outcomes. Our focus is on under-resourced communities in the especially vulnerable Southern Louisiana region.
This is a partnered project between Lousiana State University and UCLA funded by the National Academies of Science and Robert Wood Johnson Foundation. Dr. Benjamin Springgate at Louisiana State University is the overall Principal Investigator (PI) and I'm the PI for UCLA. Community Resilience Learning and Collaborative and Research Network (C-LEARN) is about better understanding the capacity to address resilience to disasters, hurricanes, storms, floods, oil spills and other natural or man-made catastrophes. We use community-partnered participatory research (CPPR) to engage stakeholders and evaluate effects of interventions on community and individual outcomes. Our focus is on under-resourced communities in the especially vulnerable Southern Louisiana region.
This project is unique in that we will work with stakeholders to randomize whole communities to a participatory-supported coalition model compared to providing technical assistance and resources. In addition, we will conduct indivudal-level randomization of a novel, mobile tool built on Chorus and co-created with community partners to support resiliency. References Consultation-Liaison Psychiatry: Telehealth and technology-enabled services

Consultation-Liaison (CL) psychiatry supports primary teams (such as medicine and surgery) caring for patients in the inpatient medical setting. Individuals are admitted for a medical reason but require assistance related to mental health. One of the challenges in CL psychiatry is matchine expertise and resources with demand for services which can be very variable. As director of the service, I worked with hospital leaderhship, doctors and nurses to help implement telemedicine for CL services. We can now conduct virtual visits via video throughout the hospital. Of course, we created a mobile app as well using the Chorus platform to help manage the CL team and activities. With telemedicine, we then explored new ways of connnecting psychiatrists with real-time requests for services at the hospital. This "on-demand" approach of enagaging a virtual pool of psychiatrists at different locations is also described in the reference below. Development is ongoing and we have since created an interdisciplinary team with psychiatric social workers to work with the psychiatrist to provide full-spectrum support for primary teams and patients at the hospital. References
My Wellness App: Participatory development of a mobile tool to support palliative care
In partnership with Dr. Thomas Strouse at UCLA, we are currently creating through a participatory development process a mobile tool to support palliative care. The process involves palliative care providers, oncologists, patients, and community partners. Using Chorus, we have developed over a series of workgroups a tailored mobile tool to help improve communication of patient and cargiver priorities and symptoms to providers and improve support at home through infomration and resources in the app. We will be conducting a pilot of this app in UCLA palliative care clinical settings soon! |

